
These slight fluctuations in the tissue's threshold And even as high as 1.25 volts at 0.4 milliseconds. Then it might go up to 1 volt at 0.4milliseconds, down again to 0.75 volts at 0.4 milliseconds. It's 0.7 volts at 0.4 milliseconds, here.
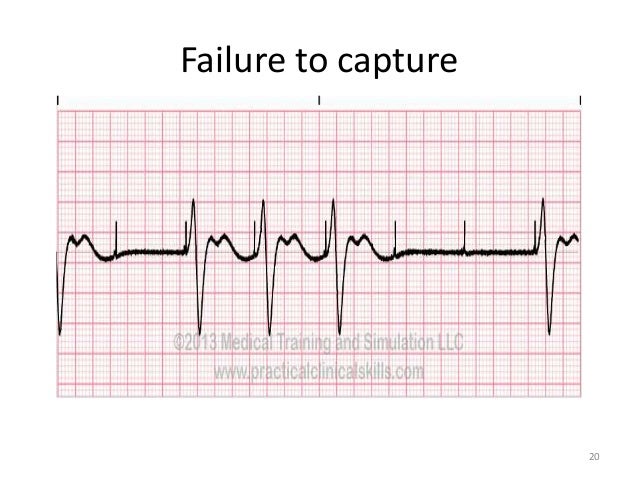
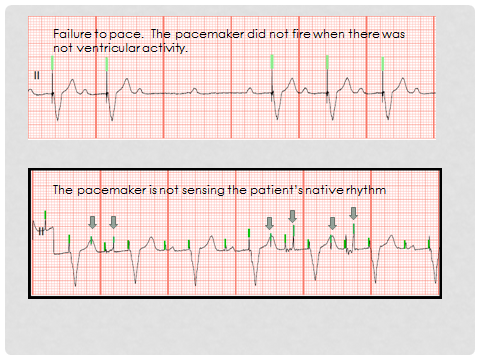
And we can see actually that in the real world, the threshold does fluctuate. They're hypothetical values for the minimum amount of energy required to trigger a depolarization in the atria When we program an output pulse, we find the threshold of the tissue and we make sure the output pulse is twice as large as the minimum amount of energy required to trigger a depolarization. So what is happening? When a pacemaker is delivering an output pulse, but it is failing to have an effect this is usually a very bad sign and I'd like And here, I've just marked on for clarity, all those events where the pacemaker has failed to capture. actually, all of these output pulses, they're represented by these pacing spikes, fail to trigger a ventricular depolarization. And on the ECG example below, we can see that, You can also have permanent or absolute or chronic failure to capture. When some of the output pulses are successful but some aren't successful, this is intermittent. However, if we look at a few heartbeats along the ECG, we can see that this output pulse has failed to trigger a ventricular depolarization. Here, we can clearly see that the output pulse, which is represented by this pacing spike has triggered a ventricular depolarization and that is what we would usually expect to see. Failure to capture is when the output pulse from the pacemaker fails to make the target chamber depolarize. This chapter will ensure that you do not fall Why is this so important? Well, I've known unnecessary surgeries to resolve problems that actually could have been solved with a small programming change. In many cases, a tweak to the programming is sufficient.
#FAILURE TO CAPTURE PACEMAKER HOW TO#
In this chapter, you will learn how to recognize the most common problems that occur and how they can be resolved. You believe the pacemaker provided a stimulus but depolarization did not occur.Now, I wish the pacemakers were infallible and once implanted, they never went wrong. Question 6: Upon assess your patient’s ECG, you notice there are pacer spikes without constant QRS complexes. You believe the pacemaker provided a stimulus but depolarization did not occur.

You believe the pacemaker identified the P wave was an extra electrical activity causing the pacemaker not to fire. Question 5: Upon assess your patient’s ECG, you notice there is a P wave without a QRS complex after. Question 4: Upon assess your patient’s ECG, you notice there is a failure to recognize the intrinsic rhythm resulting in a pacer spike falling close to another beat. Question 3: True or False: Dual chamber pacemakers will exhibit pacer spikes only before the Q wave. The nurse assesses the cardiac rhythm as: You notice a pacer spike prior to each Q wave.The overall heart rate is 80 beats per minute.
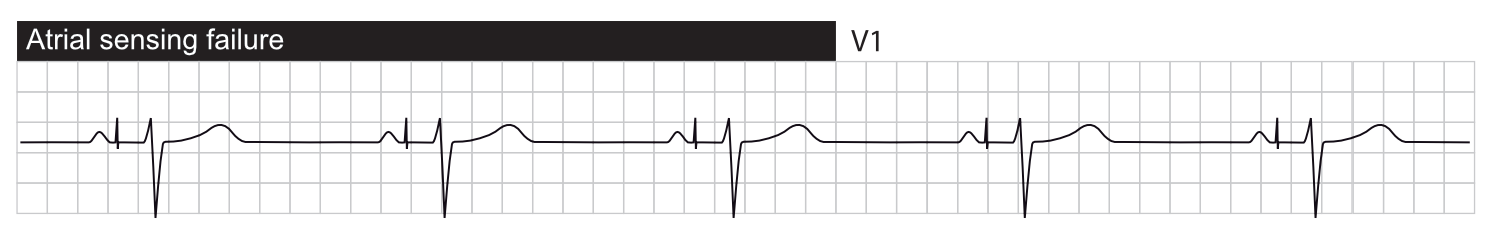
The PR interval is not measurable, and the QRS complexes are 0.16 seconds. The P waves and QRS complexes are regular. Question 2: You begin your shift and assess an electrocardiogram rhythm strip. You notice a pacer spike prior to each p wave.The overall heart rate is 80 beats per minute. The PR interval is 0.12 seconds, and the QRS complexes are 0.10 seconds. Question 1: You begin your shift and assess an electrocardiogram rhythm strip. Understanding Pacemaker Rhythms Cardiac Review – Slides Understanding Pacemaker Rhythms Cardiac Review – Notes


 0 kommentar(er)
0 kommentar(er)
